The Affordable Care Act (ACA) was signed into law in the US by then-President Obama in 2010. Many of the health insurance changes made possible by the ACA are particularly important for women living with HIV.
It is important to note that, as of this writing, the ACA is still in effect, despite high-profile attacks and repeated efforts to weaken the law by certain lawmakers and the previous US administration. The previous administration also attempted to revise various provisions of the ACA, as well as rules regarding healthcare rights, in order to limit or deny access to healthcare for certain members of the US population, such as immigrants and transgender people. Current President Biden is reversing some of these changes, and others are being challenged in court. In June 2021, the US Supreme Court dismissed a lawsuit challenging the ACA. However, other lawsuits have been filed. A lower court has decided that some preventive medications, such as PrEP, do not need to be covered, but that decision is being appealed. It may be a good idea to check online for possible recent changes in healthcare access since this fact sheet was last updated, and whether or not these changes are in effect.
Why is the ACA important for women living with HIV in the US?
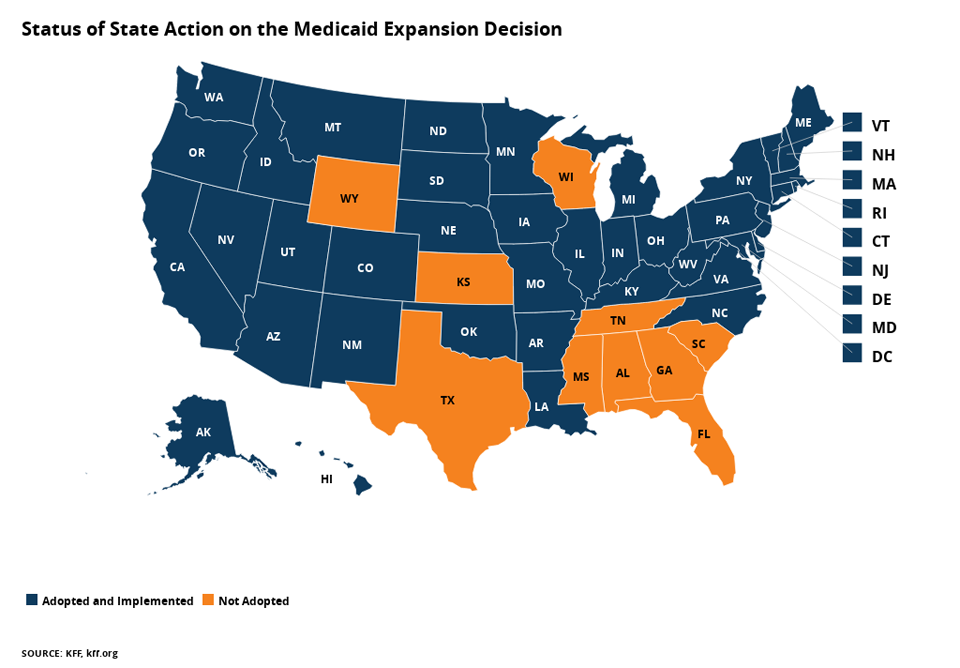
Many states have chosen to expand their Medicaid coverage, making it easier for low-income women living with HIV to get access to care.
In the past, people living with HIV had a difficult time getting access to the care and treatment they needed for HIV. They were often charged higher rates, and some were denied coverage altogether because they were living with HIV. The ACA stops insurers from denying coverage and charging higher rates for those with pre-existing conditions such as HIV.
Before the ACA, people living with HIV and with low incomes had a more difficult time accessing Medicaid. Medicaid is funded jointly by federal and state governments and handled separately by each state. This government program provides health insurance coverage to low-income people. However, many people living with HIV who have low incomes did not qualify because people needed to be both low-income AND fit into one of several qualifying groups (e.g., pregnant women, children, parents with dependent children, and people with disabilities) to be eligible for Medicaid.
Because of these requirements, many low-income women living with HIV who did not have children unfortunately had to get a diagnosis of AIDS in order to be considered disabled and qualify for Medicaid. Many states have chosen to expand their Medicaid coverage, making it easier for low-income women living with HIV to get access to care. However, some states, including several with the highest numbers of people living with HIV, have chosen not to expand their Medicaid coverage.
Women often feel the burden of health care costs more than men. Generally, women earn less than men. In addition, many women living with HIV have children or others living in their household who need care. It does not help matters that insurance companies have often charged women more than men for the same health insurance and have been able to list pregnancy as a pre-existing condition (also a cause for charging more or refusing coverage altogether). The combination of these factors has made it especially difficult for women living with HIV to get the care and treatment they need to stay healthy.
The ACA provides for several changes that can dramatically improve the health of women living with HIV. These include:
Increasing access to care
The ACA:
- Lets states provide access to Medicaid for people living below 138 percent of the federal poverty level. In addition, Medicaid eligibility is now determined based on income alone; you no longer must be disabled to qualify. In 2012, however, the United States Supreme Court ruled that it was unconstitutional to require states to expand their Medicaid coverage. Therefore, states can choose whether or not to expand coverage.
As a result, only some states have chosen to change their Medicaid eligibility requirements based on the ACA. Many of the states that have decided not to expand Medicaid are also those with the highest numbers of people living with HIV.
- Provides marketplaces or exchanges in their state to people without employer-sponsored insurance or Medicaid access to affordable health insurance where they can buy health insurance. For those who have trouble paying, federal tax credits and subsidies (money the government gives you) make the insurance premiums more affordable. Temporary additional subsidies during the COVID-19 pandemic have ended in many places.
- Stops insurers from denying coverage to those with pre-existing conditions (e.g., HIV, pregnancy, history of domestic violence)
- Prevents insurers from charging more because you are a woman
- Stops insurers from putting lifetime or annual spending limits on insurance benefits, which often affect those living with long-term illnesses like HIV
- Helps to close the "doughnut hole:" the ACA was expected to gradually close the gap in Medicare's prescription drug benefit (Part D) known as the "doughnut hole" by 2020. The doughnut hole refers to the amount between total drug costs (what you and your plan spend on medications) and a person's total out-of-pocket spending maximum for the year (this includes any co-pays, co-insurance, and deductibles). In addition, AIDS Drug Assistance Program (ADAP) payments for prescription drugs are now considered contributions toward the True Out of Pocket Spending Limit (TrOOP) for Part D, which means that people can move through the doughnut hole more quickly. In 2023, the hole still exists, but can be closed for certain low-income people through a program called "Extra Help". See the Medicare website for more information on that program.
Preventive care
Preventive care refers to tests and screenings that help us find problems early and prevent more serious diseases down the road. Many of the "preventative" tests and types of care only affect women – for example, cervical cancer screenings (e.g., pap smears), mammograms, and prenatal care for pregnant women.
The ACA requires that all new insurance plans (those beginning on or after August 1, 2012) cover the following services with no cost-sharing (no co-pay and no deductible):
- All methods of birth control approved by the US Food and Drug Administration (FDA), including the pill and the IUD. It is important to note that group health plans sponsored by employers who object to birth control for religious or moral reasons do not have to cover birth control. This exemption includes some hospitals and universities, as well as private employers.
- Annual 'well-woman' visits. This means a once-a-year gynecological exam that includes a cervical cancer screening test (e.g., a pap smear). This is especially important for women living with HIV, since they are at increased risk for cervical cancer. Studies have shown that almost one in four women living with HIV in the US does not get her recommended yearly Pap test.
- Testing for the human papilloma virus (HPV), the virus that can cause cervical cancer
- Screening for gestational (during pregnancy) diabetes for pregnant women, as well as breast pumps and counseling on breastfeeding
- Screening and counseling for domestic violence survivors. Research shows that women living with HIV are twice as likely to have experienced domestic violence compared to US women as a whole. In addition, women living with HIV who have experienced recent trauma are much less likely to be able to negotiate safer sex and to successfully control their HIV. Being able to identify and help women experiencing gender-based violence will be a huge step toward greater health for women living with HIV.
- Testing and counseling for HIV and other sexually transmitted infections (STIs)
- Mammography screening every one to two years for women over 40 years of age
- Depression screening and alcohol abuse screening and counseling. Any type of substance abuse may reduce a woman's adherence to her HIV drugs and may increase the chances that she will engage in unsafe sex. Women living with HIV are also more likely than women in the general population to experience depression. Depression can cause women to seek care less often, not take their HIV drugs as prescribed, and have their HIV get worse faster.
- Certain recommended vaccinations for children (e.g., Measles, Mumps, Rubella vaccine) and adults (e.g., annual flu shots, human papillomavirus vaccine)
A rule issued by the previous administration in 2019 allows healthcare providers to discriminate based on their religious beliefs. As of May 2021, the US Department of Health and Human Services says it will enforce the ACA non-discrimination clause, but allow exemptions based on the "Religious Freedom Restoration Act". As a result, people may be unable to get some, or all, of the health services listed above.
You can learn more about how the ACA affects women living with HIV by looking at our list of additional resources. In addition, you can go to www.healthcare.gov to find insurance options, explore the insurance marketplace, learn about prevention and wellness benefits, and find out what is changing and when.
The Well Project would like to thank Jen Kates of the Kaiser Family Foundation for her assistance with this article.

