By Gina Brown, RSW, Olivia G. Ford, and Katie Willingham
Members of The Well Project's staff and Community Advisory Board were "on the ground" March 6 – 10, 2021, at the annual Conference on Retroviruses and Opportunistic Infections (CROI 2021) – the second year the gathering has gone virtual due to COVID-19. Gina Brown and Katie Willingham were both able to attend as awardees of the competitive CROI Community Scholarship. Read on for summaries of presentations on topics of concern to our communities – and check out Gina's and Katie's blog entries about their first experiences attending the world's leading HIV research meeting.
Table of Contents
- Women's Health
- HIV and Coexisting Conditions
- COVID-19
- Systemic Inequities and Opportunities
- HIV Treatment and Prevention
- Finding a Cure for HIV
Women's Health
The following sessions addressed several key aspects of health care and life experience for many women living with HIV.
Menopause
Menopause is a normal, but often frustrating part of a woman's life. There is some evidence that women living with HIV may experience earlier menopause, and more intense symptoms of menopause, than HIV-negative women. Far more research is still needed into this important experience among women living with HIV.
"The Prevalence and Clustering of Menopausal Symptoms of Women Living with HIV" was a very interesting study that enrolled 709 women living with HIV between 45 and 60 years of age in the UK. The women chosen were from the PRIME Observational Study. The median age was 49 years old. Most (nearly 72%) were Black/African women.
The study gathered data through self-administered surveys, in which women were asked a series of questions concerning menopause and any symptoms they may be experiencing.
The following results were reported by the women:
- 30% little/no symptoms
- nearly 17% mild symptoms
- 26% moderate symptoms
- about 28% severe symptoms
The percentage of women reporting hot flashes was 63%. The women also commonly reported joint pain (a little over 66%), exhaustion (almost 62%), and sleep problems (a bit more than 61%).
The three stages of menopause – pre-, peri-, and post-menopausal – were represented in the study as follows:
- over 21% pre-menopausal
- nearly 45% peri-menopausal (transition time leading to a woman's final menstrual period)
- nearly 34% post-menopausal
They looked at clusters of symptoms according to three areas: Somatic (relating to the physical body), Psychological, and Urogenital. The study authors found that anxiety, depression, exhaustion, irritability, and sleep problems were all closely related to each other in every stage of menopause.
This was a really good presentation; more of this kind of research has to be published. – GB
Gender-Affirming Care
Medicaid is serving a critical need for transgender people with HIV in the US to access health care, and is important to ending the HIV epidemic. In 2015, New York reversed its ban on Medicaid coverage of gender-affirming care. Cristina Rodriguez-Hart, PhD, MPH, of the Bureau of HIV at the New York City Department of Health and Mental Hygiene, presented "Gender-Affirming Surgeries Accessed Through Medicaid are Associated with High and Sustained Viral Suppression Among Transgender People with HIV in New York City, 2013-2017." After an analysis of transgender people living with HIV on Medicaid in New York City, researchers found that viral suppression (very low viral load) rose rapidly from 2013 to 2017 – but was still consistently lower than among other populations.
Gender-affirming surgery may be beneficial for HIV outcomes, empowering greater self-care practices, supporting health care engagement, and allowing providers to monitor HIV clinical outcomes. Viral suppression was higher for trans people living with HIV who obtained both top and bottom surgeries as opposed to only one procedure. The study's final analysis was that gender-affirming surgery should be accessible to transgender people living with HIV regardless of ability to pay. – KW
More on this study from our partner organization POZ Magazine: Trans People Who Have Gender-Affirming Surgery Are More Likely to Have Undetectable HIV
Pregnancy and HIV Drugs
While HIV acquisition and congenital anomalies (birth defects) are important events to prevent, there are many other pressing maternal and child health outcomes to be aware of when it comes to pregnant and birthing people with HIV.
"HIV Treatment in Pregnancy: Beyond Vertical Transmission Prevention" was presented by Shahin Lockman, MD, of Brigham and Women's Hospital and Harvard T.H. Chan School of Public Health. Among other topics, Dr. Lockman spoke about:
- the need for more representation of women in research
- HIV treatment in pregnancy
- mother and child health outcomes
- differing outcomes with differing HIV drug regimens
- weight gain in HIV-negative babies born to people with HIV; and
- benefits and challenges of long-acting agents
… in addition to birth defects and reasons for new HIV cases in children. – KW
Stay tuned for a full summary of this powerful session and others relating to pregnancy, maternal, and child health!
HIV and Coexisting Conditions
The studies summarized below look at health conditions to which people living with HIV may be more vulnerable than those without HIV.
HPV and Anal vs. Cervical Pre-Cancer
Human papillomavirus (HPV) is a very common sexually transmitted infection worldwide. People living with HIV are even more likely to have HPV than their HIV-negative counterparts. High-risk strains of HPV can lead to cancers, including in the cervix and anus. Women living with HIV are also vulnerable to HPV-associated pre-cancer and cancer in these areas of the body. Cervical cancer is a recognized risk among women living with HIV, and is among the few AIDS-defining conditions specific to women. However, there are few clear recommendations for anal cancer screening or treatment among women living with HIV, though HIV guidelines note the importance of such screenings.
Were women living with HIV likely to have both cervical and anal HPV (coinfection), or was one or the other more common? Were the same HPV strains (concordance) or different ones present in the two areas? Was HPV still present over time (persistence) or did their bodies clear the infection on their own? And was persistence associated with pre-cancerous anal lesions? "Anal HPV Concordance and Persistence: Role in Anal Tumors in Women Living with HIV" explored these questions looking at a cohort of 144 cisgender women living with HIV who underwent anal HPV screening in a large urban hospital system's screening program.
Authors found that, at first screening, 45% of the women had high-risk anal HPV by itself, and 28% had anal/cervical coinfection. Of those with coinfection, 56% had the same HPV type(s) in both places. Of those who had anal HPV (either coinfection or by itself) at first visit, 54% still had it on follow-up (roughly a year and a half) and 46% cleared the infection. Pre-cancerous anal lesions were found via biopsy in 31% of the cohort. These were associated with persistent high-risk anal HPV, but not with cervical HPV.
Only 3% of this cohort had high-risk cervical HPV alone. In brief, anal HPV infection may be more common than cervical infection. Increasing screening for it among women living with HIV is likely necessary, whether or not the woman has cervical HPV. – OGF
More on this study from our partner organization TheBody / TheBodyPRO: Anal Cancer Screening Must Include Women Living With HIV, Researchers Say
Heart Problems and Sleep
Women and men living with HIV are at increased risk of heart and blood vessel (cardiovascular or CVD) problems. What factors contribute to these higher rates? Is it HIV drugs or inflammation constantly "turned on" in the body by HIV itself? Higher rates of smoking in our community? Greater likelihood of experiencing stigma, oppression, violence, and other forms of trauma – which can also increase inflammation in the body?
The answers vary depending on the person – and one factor may be sleep, or lack thereof. Sleep issues are associated with higher risk of CVD, and 70% of people living with HIV report sleep problems – especially short sleep (defined as less than seven hours per night). The study "Insufficient Sleep is Associated with Lower Endothelial Vasodilator Function in Adults Living With HIV-1" looked at 32 people living with HIV (a little under 19% female) and taking HIV drugs. The individuals in the study were free of obvious conditions that can lead to CVD or metabolic diseases like diabetes. Half of subjects in the study (two of them women) reported getting roughly 5.5 hours of sleep per night, while the other half (including the remaining four women) averaged more than seven hours of sleep nightly.
Study authors found that consistent short sleep related to lower blood vessel widening (vasodilation) in people living with HIV – and that part of the cause of that worse vessel functioning was oxidative stress. Oxidative stress (imbalance of some of the processes in the body that help keep you healthy) can interfere with the mechanism that helps blood vessels widen and keep blood flowing through the heart and body. Lack of sleep can increase oxidative stress, and lower blood vessel dilation increases risk of diseases of the heart and vessels. – OGF
More on this study (including video) from our partner organization, TheBody / TheBodyPRO: Sleep and Diet: Don't Underestimate Their Importance for People Living With HIV
Other Health Challenges and the Brain
Cognitive (thinking) impairment is more common among people living with HIV than in the general population, and is associated with worse health outcomes and lower quality of life. The CHARTER study is a large project started more than a decade ago to look at whether potential brain effects of HIV are well controlled in the era of effective, much less toxic HIV drugs. Investigators from that project retested 397 of the original participants for cognitive change 12 years after they were originally tested. No other HIV study has looked at cognitive change over this long a period of time.
At their 12-year visits, these participants ranged in age from 33 to 81. Nearly a quarter (24%) were women, and more than half (58%) were nonwhite. While nearly 75% of the group was taking HIV drugs at their first visit, that number jumped to 96% 12 years out. This group also experienced notable increases in conditions like diabetes (from under 7% to 20%) and hypertension (from nearly 19% to nearly 49%) over the 12 years, which was not considered unusual given the average age of the group was 56. Interestingly, the group reported less depression than they did 12 years before.
Participants went through tests of seven cognitive categories, as they did 12 years prior – including motor ability, speed of information processing, and working memory. Cognitive decline was found in nearly a quarter of participants, though it is important to stress that the extent of decline was not serious in most participants. Worse change was associated with aging-related conditions that had already been identified as risk factors (such as diabetes), but was also associated with other risk factors that have not been considered in this way before (like chronic lung disease, major depressive disorder, and excessive, problematic cannabis use).
Taking a high blood pressure drug (antihypertensive) was associated with less cognitive decline. Further, study authors saw worse change among people who had high blood pressure at their first visit and were not taking a drug for that condition at their second visit. – OGF
COVID-19
Since the start of the COVID-19 pandemic, numerous HIV researchers have turned their expertise toward learning more about COVID-19 - both by itself and in relation to HIV. The presence of many COVID-19-focused sessions and studies at CROI 2021 reflects this reality.
The speaker in the COVID-19 session that I found most impressive was Galit Alter, PhD, of the Ragon Institute of Massachusetts General Hospital (MGH), MIT, and Harvard. She spoke about "Advances in HIV and SARS-CoV-2 Immunology." I learned why vaccines are so much harder to make for HIV than SARS-CoV-2 (the virus that causes COVID-19). I also learned how immune activation, lower CD4 T cells, exhausted T-cell immunity, poor B-cell immune responses, and compromised innate immunity contribute to HIV remaining deadlier than SARS-CoV-2. As Dr. Alter noted, HIV has at least a 95% death rate without treatment and accounts for 75 million cases and 35 million deaths since its beginning almost 40 years ago – while SARS-CoV-2 has amassed 2.6 million deaths out of 116 million cases (as of her presentation) in just one year, which is also horrific.
Dr. Alter also pointed out another difference between HIV and SARS-CoV-2. With HIV, people may experience symptoms in the weeks after acquiring the virus, when there is a high level of viral replication (virus making copies of itself) in the body, and then have no symptoms for many years. With SARS-CoV-2, there is almost a "switch" in which symptoms of severe disease may continue even after the virus has cleared, and continue for up to six months (or even longer, in cases of what is starting to be called "long COVID"). However, she did say that we are learning a great deal about SARS-CoV-2 vaccines that could possibly inform HIV vaccine research.
Jurgen K. Rockstroh, MD, of Medizinische Universitatsklini spoke about "Advances in COVID-19 Treatment Strategies and Controlling the Epidemic." He talked about lessons learned from easing COVID-19 restrictions, testing basics, therapeutic management of patients with COVID-19, and a variety of developing treatments. He was very optimistic; however, when asked, he said that he thought that COVID-19 was endemic and would be around for a long time. – KW (with OGF)
At the first morning science review breakfast of the conference, Gregg Gonsalves, PhD, a longtime HIV advocate, led a discussion about COVID-19 vaccine nationalism, issues of vaccine production, inequities of distribution, the threats of variants of the virus, and vaccination passports. He gave a call to action against vaccine inequity: the fact that most of the vaccine is going to the richest countries who often have enough vaccine to vaccinate their citizenry two or three times, while much poorer countries are forced to wait. Talking about the role of advocacy in a pandemic, he said: "It's not fair that HIV advocates must take up another pandemic, but we can do it."
During the Martin Delaney Presentation (an annual event at CROI), Jim Pickett moderated a discussion between Gonsalves and Fatima Hassen of Health Justice Initiative, Cape Town, South Africa. Their conversation was titled "Vaccine Nationalism Is Killing Us: How Inequities and Access To SARS-CoV-2 Vaccines Will Perpetuate the Pandemic." These two powerful speakers were engaging and informative. Gonsalves laid the foundation with a quote by Larry Kramer: "AIDS is about disposable people." If you think about it, so is COVID-19. The same people that bear the brunt of HIV, both in the Global South and the US South, are also disproportionately impacted by COVID-19.
Hassen reported that situations are dire in the Global South, as 130 countries have limited access to vaccines and governments and pharma aren't doing enough to help. She painted a clear picture of the needs of health care workers in the Global South to get a COVID-19 vaccine. Gonsalves said, "We've learned from AIDS what happens when you don't confront a pandemic early."
Now is not the time to leave anyone out of the fight to prevent COVID-19. The only way this pandemic will end is by everyone having equal access to a COVID-19 vaccine. Which brings me to another point: People living with HIV must continue advocating for a vaccine for HIV. After the speed in which we identified a viable COVID-19 vaccine, we should be able to discover an HIV vaccine in my lifetime.
Sign the Call for Global Vaccine Equity
– GB and KW
The N'galy-Mann Lecture (another annual event at CROI) was delivered by Anthony Fauci, MD, longtime director of the National Institute of Allergy and Infectious Diseases and chief medical adviser to President Joe Biden. Dr. Fauci spoke about lessons learned from the concurrent HIV/AIDS and SARS-CoV-2 pandemics. He talked about five specific areas: epidemiology/natural history, non-vaccine prevention, vaccine prevention, efficacy versus effectiveness, and denialism. He talked about how epidemics exacerbate health disparities, particularly along racial/ethnic lines and how communities disproportionately affected by disease must engage in research and advocacy, as advocacy plays a role in science. – KW
New Weapons to Fight COVID-19
Myron S. Cohen, MD, of The Institute of Global Health and Infectious Diseases of The University of North Carolina at Chapel Hill presented "Bamlanivimab Prevents COVID-19 Morbidity and Mortality in Nursing-Home Setting." He presented on BLAZE-2, which is an ongoing, phase 3, randomized, double-blind, placebo-controlled, single-dose study that found that bamlanivimab (a monoclonal antibody given through an IV infusion) was safe and effective in significantly reducing COVID-19 in assisted living facilities. This study is important because it shows the ability of a monoclonal antibody to prevent SARS-CoV-2 infection and to prevent progression of COVID-19 in high-risk populations.
Meagan P. O'Brien, MD, of Regeneron Pharmaceuticals, Inc. presented on "REGEN-COV Antibody Cocktail of Casirivimab with Imdevimab for COVID-19 Prevention: Interim Results." She described an interim analysis of a phase 3, randomized, placebo-controlled study of 409 people who did not have COVID-19, with promising results: A cocktail of casirivimab and imdevimab (REGON-COV) resulted in 100% prevention of symptomatic cases and 100% prevention of infections with high viral load in participants who got the study drug. Treatment also resulted in ~50% lower overall rates of infection (both symptomatic and asymptomatic) and was well tolerated. REGEN-COV also decreased the period of time that a person was likely to transmit the virus to others. – KW
Systemic Inequities and Opportunities
It is well documented in HIV-related literature that unequal social conditions fuel the HIV epidemic far more than individual people's behavior. COVID-19 has only made worse those dangerous inequities. CROI 2021 brought together top minds in this area to discuss what can be done to eliminate these conditions.
"Disparities in COVID-19 Among Racial and Ethnic Minorities in the US" was presented by Mary T. Bassett, MD, MPH, of Harvard T.H. Chan School of Public Health. She spoke about the effects that race and racism have had, historically in the HIV response and likewise in the response to COVID-19, how disparities have appeared quickly and across not only race but also age, including people of color being affected at much younger ages than white people. These disparities create greater rates of morbidity and mortality along with lower rates of vaccination and trust. She concluded that we must address societal and health system vulnerabilities and commit to an equitable response.
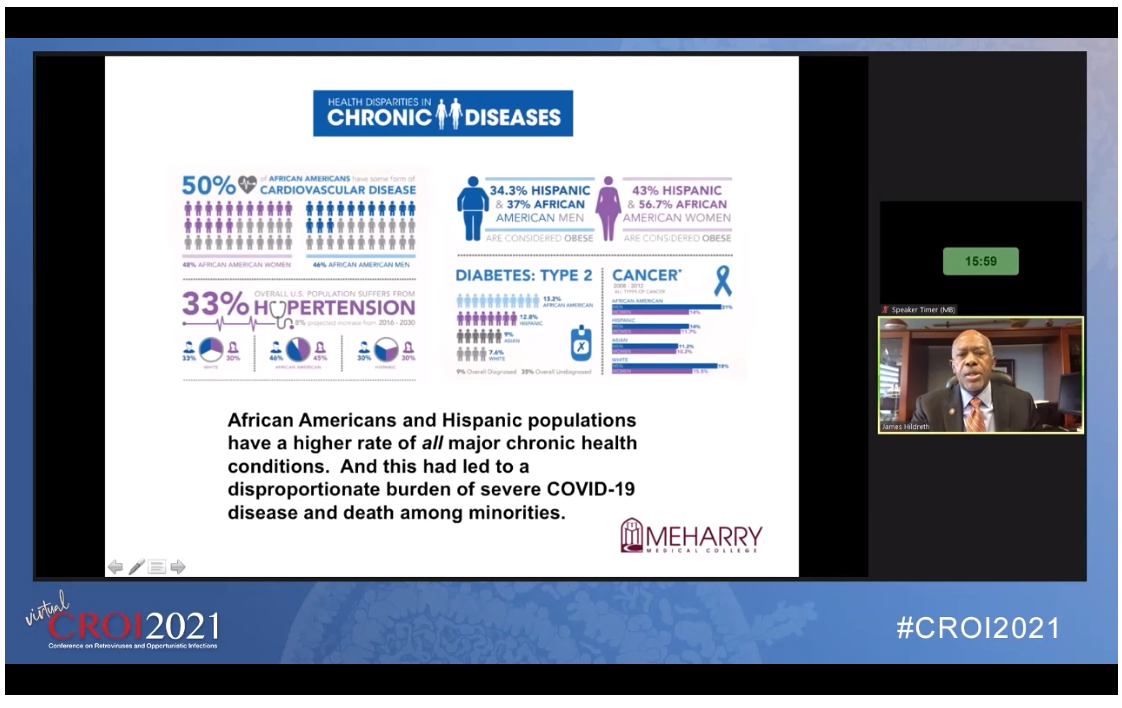
James E. K. Hildreth, MD, PhD, president and chief executive officer at Meharry Medical College, talked about “Disparities in Health: From HIV to COVID-19 and Beyond.” He spoke about the stigma and discrimination that have affected people living with HIV from the start of the pandemic (which, in the beginning, was referred to as Gay-Related Immune Deficiency) and how those disparities have particularly affected communities of color and blocked effective responses.
He then moved on to COVID-19 and discussed how neglect and negative rhetoric have similarly hurt the response to this pandemic, and have once again mostly harmed communities of color who have higher rates of comorbidities and more challenging social determinants of health. He elaborated on five social determinants of health, how to address them, and the need to transition from health disparities to health equity. – KW
"Geographic Differences in Time to Viral Suppression in the Deep South" was presented by Aadia Rana, MD, of the University of Alabama at Birmingham. She spoke about the importance of achieving early and sustained viral suppression following HIV diagnosis to improve outcomes and reduce transmission in the disproportionately affected Deep South.
Using the time it took for participants to become virally suppressed (which captured the collective activities of prevention and care), the study found dramatic variation from place to place. While time to viral suppression remains longest in the Deep South, trends in time to viral suppression were found to be improving in Alabama, Mississippi, and Louisiana, the states where the study was conducted. Such improvements are being seen across the country, and may be due to changing guidelines recommending universal test-and-treat strategies and better tolerated treatment.
It is worth noting that the state that saw the greatest improvement in time to viral suppression was Louisiana – the only state in the study (and in the Deep South) that has expanded Medicaid in light of the Affordable Care Act. It's also vital to have academic and public partnerships to direct evidence-based interventions. Next, their team will assess the impact and interplay of individual, structural, and community level socio-contextual variables on time to viral suppression. – KW (with OGF)
HIV Treatment and Prevention
The sessions below highlight exciting developments for people living with and vulnerable to HIV.
In a pre-CROI morning session about some of the great science coming out of this year's CROI, Randy Matthews, MD, PhD, of Merck and Co. talked about injectables, implants, and long-acting agents. He described implant placements and replacement, and the ease of the procedures requiring few skills. He also explained that these approaches have the possibility of administering other, non-HIV medications, such as contraception. Reliability of injectables and implants appears good, and resistance negligible. There's great interest in trial results and further development.
Jean-Michel Molina, MD, of the University of Paris spoke about "Advances in Biomedical Prevention for HIV." He talked about vaginal gel and rings, PrEP, trials and studies and what was learned from them along with new developments in drugs like the promising development of injectables and findings showing them to be highly effective for women and vaccine development. – KW
In the oral presentation "Next-Generation Islatravir Implants Projected to Provide Yearly HIV Prophylaxis," the researcher presented data on the Phase 1 trial of islatravir, a nucleoside reverse transcriptase translocation inhibitor (NRTTI). Because of its makeup, it's suitable for long-acting delivery. Islatravir is a delayed release implant that would put medication into the body over a year. The drug properties of islatravir and its half-life of approximately 190 hours makes this drug look promising as another PrEP tool. The implant would work like the Norplant contraceptive implant, inserted beneath the skin and a certain amount of the medication is released daily.
There were 36 "low-risk" men and women in this double-blind study. This could be a real game-changer for women. Especially Black and Latinx women – the two groups that contract HIV at a higher rate than their white counterparts, yet are at the bottom for people being reached with PrEP. There may be shame associated with taking a pill daily; an implant would eliminate that shame. Although this research is in its early stages, they did see the following benefits/positive results:
- All three next-generation PrEP implants show promise in all three dosing sizes:
- 48 mg
- 52 mg
- 56 mg
- Islatravir implant is well tolerated
- A dose of islatravir >52mg was sufficient for 52 weeks
- Results from initial trial makes the case for Phase 2
– GB
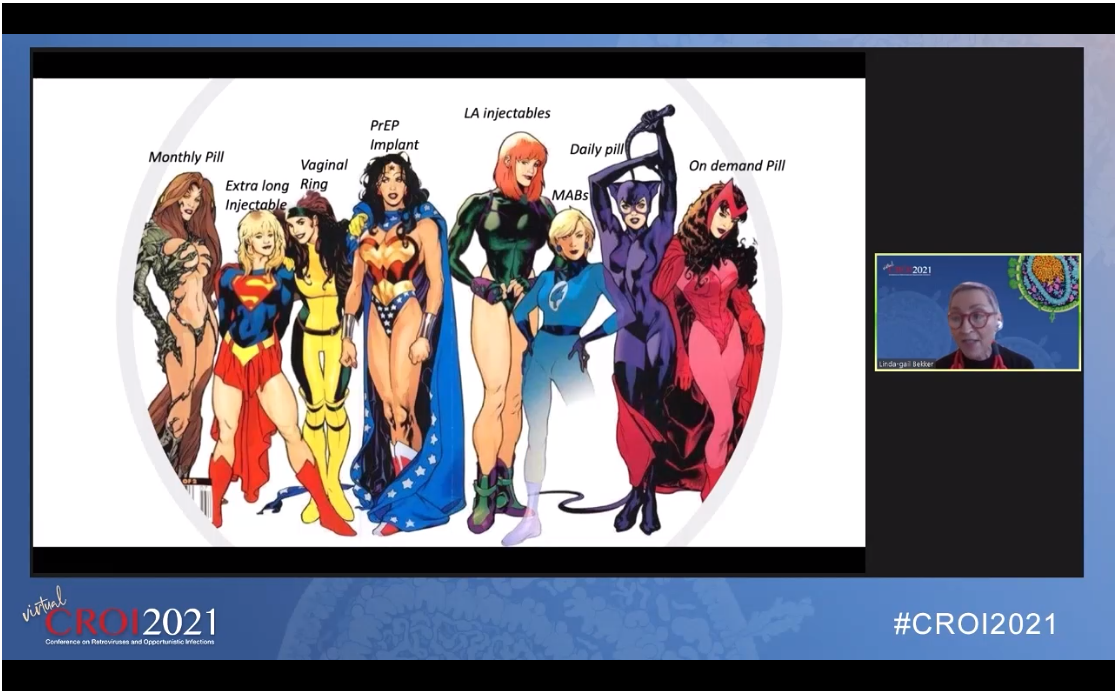
Linda-Gail Bekker, PhD, MBChB, of The Desmond Tutu HIV Centre of the University of Cape Town, presented "Sustained Delivery and Long-Acting Agents for Prevention of HIV." She talked about advances in PrEP and its impact so far, as well as its limitations as a daily regimen with its challenges of adherence, particularly in the young. Her solution is longer acting agents in different formulations for less frequent and alternative dosing, including injectables and implants which are currently under development – the "superheroes of prevention," each with their own approach and benefits.
"We as humans come in many shapes and forms, and there is no doubt that our prevention should as well," Dr. Bekker concluded. "Preference requires choice, and may vary depending on timing, circumstances, life course, and relationships." – KW (with OGF)
More on this topic (including video) from our partner organization TheBody / TheBodyPRO: CROI 2021 Takeaway: Long-Acting Antiretrovirals for HIV Treatment
Finding a Cure for HIV
The journey continues in finding ways for people living with HIV to live for long periods of time - even the rest of their lives - without regular treatment.
Marina Caskey, MD, of The Rockefeller University, presented "HIV-1 bNAbs: Looking Ahead" and spoke about the use of broadly neutralizing antibodies (bNAbs). In this approach, antibodies (proteins our bodies produce to help fight diseases) that are very good at disabling a specific virus are cloned and used to prevent or treat that virus. Now I didn't know what bNAbs were, but I know I've been hearing a lot about them in the realm of HIV cure research. Dr. Caskey outlined potential roles of HIV-1 bNAbs, lessons from SARS CoV-2 immunotherapy, HIV-1 bNAbs clinical data in prevention, therapy and cure, and advances in promising preclinical data, new technologies and delivery systems.
More on this topic (including video) from our partner organization TheBody / TheBodyPRO: Broadly Neutralizing Antibodies for HIV? If We Can Do It for COVID ...
"Elite Controllers: A Model for a Functional Cure of HIV-1 Infection" was presented by Xu Yu, MD, of the Ragon Institute of MGH, MIT and Harvard. He spoke about HIV reservoirs as an obstacle to cure, the difference between sterilizing cure (HIV completely removed from the body) and functional cure (HIV still in the body, but not active), and how persisting HIV proviruses in elite controllers differ from persisting reservoirs in people whose HIV is controlled with HIV drugs. He summarized that quality rather than quantity of viral reservoirs can be an important distinguishing feature for a functional cure of HIV.
Katharine J. Bar, MD, of the University of Pennsylvania presented on "Advances in HIV Cure." She spoke about overlapping and mutually dependent priorities to elucidate and overcome barriers to HIV cure. These priorities are to A) Define mechanisms of HIV persistence, B) Accurate reservoir measurement assays, C) Develop cure strategies and D) Empiric testing of cure strategies. She covered these priorities in some detail. – KW
More on CROI 2021 from Around the Community
- More Women … Please? by Gina Brown, RSW, on A Girl Like Me
- My First CROI, by Katil Willingham on A Girl Like Me
- The Personal is Planetary: CROI and COVID One Year On (AVAC)
- #CROI2021 on POZ.com (POZ)
- Top 5 Stories on HIV, Ageing and Co-Morbidities from CROI 2021 (aidsmap)
- Women & HIV at CROI (NATAP)
- Coverage of CROI 2021: The 28th Conference on Retroviruses and Opportunistic Infections (TheBodyPRO)
- Really Rapid Review — CROI 2021 Virtual (NEJM Journal Watch)