Table of Contents
- The Importance of Healthy Bones
- Bone Loss and HIV
- How to Know if You Have Bone Problems
- Factors Affecting Your Bone Health
- Drugs to Treat Osteoporosis
- Protect Your Bones
The Importance of Healthy Bones
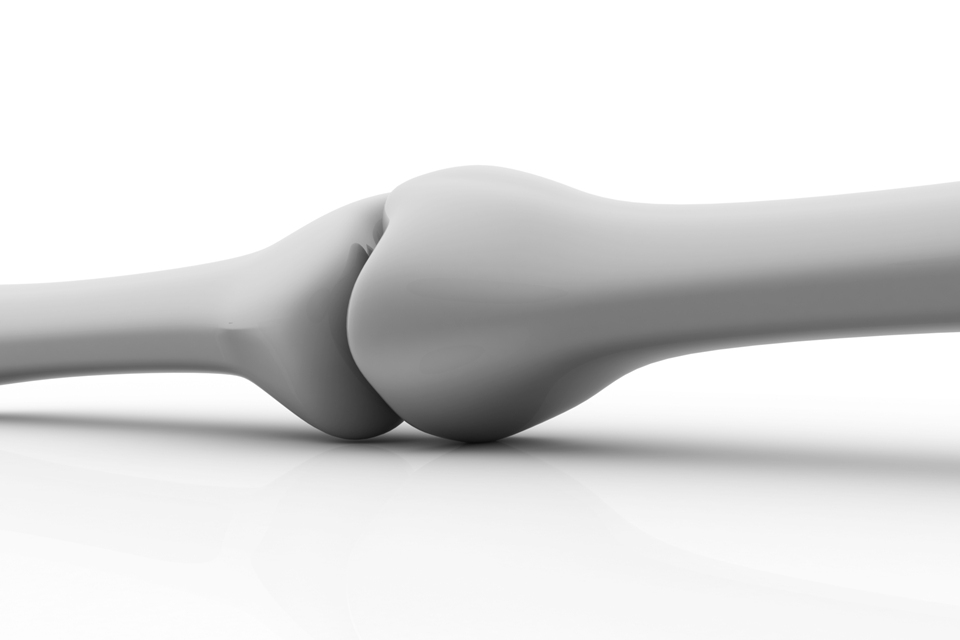
Bones play many important roles in your body. They support you, help you move, and protect some of your organs from injury. Bones also store minerals, such as calcium and phosphorus, and make many of the cells that circulate in your blood (e.g., red blood cells, white blood cells, platelets).
Bones are constantly changing throughout your life. Every day, your body removes old bone and adds new bone in its place. In young people, more bone is added than removed. After age 30, more bone is removed than added. As a result, the bones become lighter and weaker, which puts them at greater risk for injury.
Every day, your body removes old bone and adds new bone in its place.
Many people have weak bones and do not know it. This is so because bone loss often happens over a long period of time and does not hurt. For many people, a broken bone or a fracture is the first sign of weakened bones. This weakness is often referred to as low bone mass or low bone density. Bone mass or bone density refers to how much internal bone structure is in a given section of bone. For example, more dense bone has more calcium and phosphorus – two key minerals that make up bone – per square inch of bone.
Bone Loss and HIV
Bone loss and weakened bones occur more often in people living with HIV. Experts are not exactly sure why. It could be due to HIV itself, HIV drugs--or the fact that people living with HIV are living longer and experiencing more of the regular effects of getting older. People living with HIV are more likely to experience three bone conditions: osteopenia, osteoporosis, and osteonecrosis.
Osteopenia
Osteopenia is caused by a loss of bone minerals that leads to lower-than-normal bone density. Most often, osteopenia has no symptoms. The only way to know if you have this condition is to have a bone density test (DEXA scan). If you do learn that you have osteopenia, there are things you can do to stop it and possibly even reverse it (see the Physical Activity and Diet sections below).
Osteopenia can lead to a more serious condition called osteoporosis (see below). Having osteopenia does not mean you will definitely develop osteoporosis, but it does mean that you are more likely to develop it. Although bone loss with osteopenia is generally less severe than with osteoporosis, it does indicate that bones are weaker and may be more likely to break.
Osteoporosis
Osteoporosis is a more serious condition than osteopenia and refers to a loss of bone density and bone mass. Over time, breaking down more bone than is replaced causes lower bone mineral density, which means there are lower-than-normal levels of minerals in the bones. Bones become weak and are more likely to break. People with osteoporosis most often break bones in the wrist, spine, and hip. Sometimes bones break without an injury.
Osteonecrosis (avascular necrosis)
Osteonecrosis means bone death. It is caused by a loss of blood supply to the bone. Osteonecrosis may cause pain at the affected joint. It usually affects the head of the femur, the ball-shaped part of the thigh bone that connects it to the hip.
How to Know if You Have Bone Problems
Osteoporosis and Osteopenia
Bone mineral density (BMD) tests are the only way to find out if you have osteoporosis or osteopenia. The most widely used BMD test is a DEXA (Dual Energy X-ray Absorptiometry) scan. The DEXA scan is a kind of x-ray, and is an easy and painless test that takes about 15 minutes.
Osteonecrosis
Osteonecrosis can cause pain in the joints, usually in the hip area. At first, the pain may only occur when you put weight on the joint. In more severe cases, the pain can be constant. An MRI (magnetic resonance imaging) scan can spot early stages. X-rays and other scans can detect advanced osteonecrosis.
Guidelines for Bone Care
The World Health Organization (WHO) recently released new guidelines for the management of bone health among people living with HIV. The guidelines recommend that all pre-menopausal (still having their period) women living with HIV who are 40 years old or older have their risk of fracture measured using the Fracture Risk Assessment Tool (FRAX) without a DEXA scan. This assessment looks at risk factors for fracture (e.g., age, smoking, family history of fracture, etc.) and calculates a probability of future fracture.
The guidelines also suggest that DEXA scans be conducted for all postmenopausal women living with HIV, people living with HIV who have a history of fragility fracture, people living with HIV who are receiving chronic glucocorticoid treatment, and people living with HIV who are at high risk of falls.
Lastly, the guidelines recommend that people living with HIV who are at risk for bone loss and/or fracture have their HIV treatment regimens adjusted so that they do not contain tenofovir disoproxil fumarate (TDF; see Tenofovir section below).
In the US, guidelines suggest DEXA scans for everyone living with HIV who is older than 50 years and for women who are past their menopause (no longer have their periods).
Factors Affecting Your Bone Health
Stopping smoking is one of the single best things you can do for your health.
There are several things that can affect your bone health and put you at risk for bone loss. Some of these are things you cannot control:
- Age: Your chances of getting osteoporosis increase with age
- Sex: Women have a greater chance of getting osteoporosis than men
- Menopause: Women lose bone due to hormone changes that happen after menopause. While hormone replacement therapy is no longer routinely recommended, it is an effective therapy for bone loss that does not respond to other treatments.
- Family history: Having a parent with osteoporosis, especially a mother or father who has had a hip fracture, increases your risk of bone loss
The good news is that there are also several things that you can control – things that you can do to maximize your bone health, regardless of your age, sex, or family history.
Diet and Body Weight
Even though you cannot control all of the things that lead to bone disease, you can control your diet. The mineral calcium makes up a large part of your bones. This means that if you do not get enough calcium in your diet, your bones may get weaker.
Calcium is found naturally in some foods, and it is added to others. Some foods that contain calcium are:
- Dairy products, including milk, yogurt, and cheese
- Soy products: tofu, tempeh, soy milk
- Seeds: sesame seeds, chia seeds, and flax seeds
- Dark leafy greens: spinach, kale, chard, collard greens, turnip greens
- Broccoli
- Beans: black beans, navy beans
- Dried fruits and nuts: figs, almonds, Brazil nuts
- Oranges and orange juice (especially calcium-fortified orange juice)
- Salmon or sardines with the bones
Some people living with HIV still need to take calcium pills every day, even if their diet includes foods with calcium in them. A registered dietitian or other trained health care provider can help you decide whether you should take calcium supplements. If you do take calcium supplements, it may be a good idea to take calcium pills with vitamin D in them, since your body cannot use calcium without vitamin D. According to the Office of Dietary Supplements at the National Institutes of Health (NIH) in the US, the recommended dietary allowances are:
- Girls and young women nine to 18 years old need 1,300 mg of calcium and 600 IU of vitamin D daily
- Women 19 to 50 years old need 1,000 mg of calcium and 600 IU of vitamin D daily
- Women over 50 years old need 1,200 mg of calcium and 600 IU of vitamin D daily
- Pregnant and breastfeeding teens need 1,300 mg of calcium and 600 IU of vitamin D daily
- Pregnant and breastfeeding adults need 1,000 mg of calcium and 600 IU of vitamin D daily
It is important that you talk to your health care provider before taking any supplements, and not take more than these amounts unless your health care provider tells you to take more. Many first-line HIV regimens that include integrase inhibitors may not be absorbed by the body as well as they should be when they are taken with calcium supplements. It is important that you discuss with your health care provider how to take these medicines together.
Physical Activity
If you do not have joint pain, it is important to be physically active on a regular basis. When you exercise, your muscles pull against your bones, which helps keep your bones healthy and strong. The best kind of physical activity to keep your bones strong is one that uses weight or resistance such as:
- Walking (you can use ankle weights)
- Working out with weights, weight machines, or bands (also called resistance training)
- Stair climbing
- Hiking
- Aerobics
- Jogging
If you cannot do high-impact weight-bearing activities, try lower-impact ones. For example, try walking or stair climbing instead of jogging. If you have not exercised regularly for a while, check with your health care provider before beginning a new exercise program.
Once you have your health care provider’s approval, start your exercise routine slowly. Every week or two, make your routine five minutes longer. In the end, it is recommended that you do 150 minutes of moderate-level physical activity each week (e.g., five 30-minute workouts).
Tobacco, Alcohol, and Caffeine
Using tobacco products, whether it’s smoking or vaping, using snuff, or chewing tobacco, can increase your chances of bone loss. If you use tobacco, it is a good idea to try and quit. Stopping smoking is one of the single best things you can do for your health. Talk with your health care provider about stopping smoking – there are many tools to help you quit. You can also find lots of information and support online (http://www.smokefree.gov).
Drinking a lot of alcohol and/or caffeine can also put you at greater risk of bone loss.
Using Certain Medicines
Long-term use of some medicines can increase the chances of bone loss and lead to weakened bones:
- Depo-Provera (an injectable form of birth control)
- Glucocorticosteroids (drugs such as prednisone and cortisone)
- Thyroid hormones
- Anticonvulsants (anti-seizure medications)
- Heparin (blood thinner)
- Pentamidine (antibiotic)
- Ketoconazole (anti-fungal)
- Tenofovir disoproxil fumarate (TDF or Viread; see below)
Tenofovir: TDF and TAF
Tenofovir is an HIV drug that comes in two forms: TDF (tenofovir disoproxil fumarate) and TAF (tenofovir alafenamide). TDF is also known by the brand name Viread and found in other combination drugs such as Truvada (tenofovir disoproxil fumarate plus emtricitabine). TAF is not available by itself for the treatment of HIV, but is found in the following approved combination pills:
- Biktarvy (bictegravir plus emtricitabine plus tenofovir alafenamide)
- Descovy (emtricitabine plus tenofovir alafenamide)
- Genvoya (elvitegravir plus cobicistat plus emtricitabine plus tenofovir alafenamide)
- Odefsey (emtricitabine plus rilpivirine plus tenofovir alafenamide)
- Symtuza (darunavir plus cobicistat plus emtricitabine plus tenofovir alafenamide)
For more information on these HIV drugs, see our HIV Drug Chart.
Previous studies have shown that treatment with TDF can lead to lower kidney function and bone loss. Treatment with TAF has been proven to not only produce less bone loss and less reduction in kidney function, but to improve existing kidney and bone problems in those who switched from TDF. TAF can be given at lower doses than TDF while achieving the same level of HIV suppression.
A study of over 12,000 Europeans living with HIV found that treatment with TDF increases not just bone loss, but the risk of actual bone fracture in adults. This is an especially important consideration for women, who often experience bone loss naturally after menopause. The risk of fracture did not increase with increasing time on TDF, which matches our understanding that most of the bone loss associated with taking tenofovir disoproxil fumarate occurs early in treatment.
Drugs to Treat Osteoporosis
Diet and exercise are best for keeping bone loss from occurring. They can also be helpful if you already have osteopenia or osteoporosis, but in some cases your health care provider may also recommend treatment with medication.
Make sure to ask your health care provider about how to take the medication, possible side effects, and whether there are any interactions with HIV drugs you take. Some of the osteoporosis medications that are commonly used include:
Bisphosphonates
These drugs are widely used to treat and prevent osteoporosis. They include:
- Fosamax (alendronate)
- Boniva (ibandronate)
- Actonel or Atelvia (risedronate)
- Zometa, Zomera, Aclasta and Reclast (zoledronic acid)
It is important to get enough calcium and vitamin D when you are taking a bisphosphonate.
Hormones
- Estrogen: In women, replacing the hormone estrogen has been shown to decrease the number of fractures. Sometimes estrogen is combined with another hormone called progesterone. However, estrogen replacement therapy can increase the risk of developing other diseases, including certain cancers. Because of this, the US Food and Drug Administration (FDA) recommends using other osteoporosis medications. If estrogen/progesterone are used, the lowest possible doses should be considered.
- Testosterone: Testosterone therapy may be useful to slow or reverse decreased bone density and strength in men
- Miacalcin (calcitonin): This naturally occurring hormone slows bone loss and increases bone density in the spine
- Teriparatide (Forteo), abaloparatide (Tymlos) and romosozumab (Evenity): These parathyroid hormones have been shown to rebuild bone and increase bone mineral density, especially in the spine
Selective Estrogen Receptor Modulators (SERMs)
Evista (raloxifene) is in a class of osteoporosis drugs called SERMs. It was developed to work like estrogen therapy, but with fewer side effects.
Bone-Modifying Agent, a Monoclonal Antibody
Denosumab (Prolia or Xgeva) is given as a shot (injection) and is used to treat postmenopausal women at high risk for fracture. It works by stopping the development of cells that remove bone.
Protect Your Bones
It is important that women living with HIV, especially those who have experienced menopause, pay careful attention to their bone health. Speak to your health care provider and follow these steps to help protect your bones:
- Ask your health care provider if you need a DEXA scan
- Follow a diet with plenty of calcium and vitamin D
- Seek the advice of a registered dietitian if you need help choosing the right foods
- Take calcium supplements if needed (talk to your health care provider first)
- Ask your health care provider what physical activity is safe for you, and start doing it
- Stop smoking and reduce your intake of caffeine and alcohol
- Tell your health care provider if you are experiencing joint pain, especially in the hip area