
Lea esta hoja informativa en español
Note: In this fact sheet, "woman" and "man" refer to cisgender people. Much of the information for "women" is relevant to people assigned female sex at birth who do not identify as women; and the information for "men" is relevant to people assigned male sex at birth who do not identify as men.
There are several different options for reducing the chances of passing on a different strain of HIV while trying to conceive (get pregnant; have a baby). If you are a woman living with HIV and a man living with HIV, the options below can help you understand what might be best for you and prepare for discussions with your healthcare provider(s) and others. (For other options and more general information, you can return to the main "Getting Pregnant and HIV" page.)
Viral Suppression of Partners Living with HIV
One of the best things that you both can do in this situation is to take HIV drugs regularly and maintain a suppressed viral load, even when you have no symptoms and a relatively healthy immune system. This will reduce the possibility of passing a different strain of HIV (one that may be stronger or more drug-resistant) to your partner. Transmitting a different strain of HIV to a partner who is already living with HIV is called "superinfection."
As with serodifferent partners, you can reduce the risk of passing HIV to your baby or a different strain of the virus to your partner by reducing your viral load before trying to become pregnant. Having an undetectable viral load lowers transmission risk to a baby to less than 1 percent. Screening and treating any sexually transmitted infections or diseases (STIs or STDs) before trying to get pregnant will also lower your chances of passing a different strain of HIV between partners.
Condomless Sex
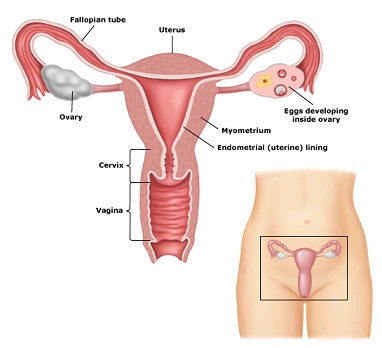
If you choose this method, the chance of getting pregnant is higher if you have condomless sex when the woman is ovulating (when she is most likely to get pregnant; this is often called 'timed intercourse'). Ovulation occurs when an egg is released from the woman's ovary and usually happens about two weeks before a woman starts her menstrual period. Insemination during the "fertile window" – usually one to two days before ovulation until one day after ovulation – has a greater chance of success. For more information on understanding and tracking your fertility, visit:
Home Insemination with Donor Sperm
This involves using donor sperm from someone you know or from a sperm bank. Not all states allow sperm from a sperm bank to be used for home insemination. If using donor sperm from a sperm bank for home insemination is possible in your state, ask your sperm bank for instructions on how to use the sperm at home.
If using sperm from someone you know, have the man ejaculate (cum) into a clean cup or condom. If using a condom, be sure to use one without spermicide. Then, using a syringe (without a needle), you suck up the semen and insert the syringe deep inside the vagina. Once the syringe is deep inside the vagina, you squeeze out and deposit the semen.
Based on individuals' experiences and at least one study, it is often recommended that the woman lie down for 20 minutes after inserting the semen to improve fertility. It is also more effective to use home insemination when a woman is fertile, or when she is ovulating. You can get non-needle syringes at most any pharmacy because they are commonly used to give medicines to babies. Your HIV provider may also have some to give to you.
Sperm Washing
Sperm washing refers to a process in which sperm is separated from seminal fluid (semen = sperm + seminal fluid). Since HIV exists in seminal fluid but not in sperm, 'washing' the sperm clean of the seminal fluid lowers the risk of HIV transmission. See "Understanding the Science" for more information. Washed sperm can be used with the assisted reproductive techniques described below.
Assisted Reproduction
This means that a sperm fertilizes an egg with the help of a medical technique or therapy. Assisted reproduction (sometimes called "assisted reproductive technology") is useful when the future parent(s) require help to prevent HIV transmission between partners, are using donor sperm, or are having difficulty getting pregnant at home because of fertility issues. Unfortunately, few facilities offer assisted reproduction to people living with HIV, and few health insurance plans cover it. There are several types of assisted reproduction:
- Intra-vaginal insemination (IVI): Very similar to home insemination, only done in a clinic.
- Intra-uterine insemination (IUI): Sperm is drawn up into a narrow tube, which is then inserted through the cervix into the uterus (womb). The sperm is deposited in the uterus, where fertilization of the egg can occur.
- In-vitro fertilization (IVF): The woman takes fertility drugs to help her prepare eggs (also called ripening her eggs). When eggs are ready (or ripe), they are removed from the ovary and put in a dish with sperm. Once there is a fertilized egg (embryo), it is put back in the woman's uterus.
- Intra-cytoplasmic sperm injection (ICSI): This is a specific type of IVF in which a sperm is injected directly into an egg using a very thin needle. When a fertilized egg occurs, it is returned to the woman's uterus. This method is used when a man's sperm do not swim well or are not normally shaped.
Egg Donation
This involves using IVF and eggs donated by another woman, who is checked for fertility and diseases. The woman who is donating eggs takes fertility drugs to help her prepare eggs (also called ripening her eggs). When eggs are ready (or ripe), they are removed from her ovary and put in a dish with sperm. Once there is a fertilized egg (embryo), it is put in your womb (uterus). Although this method uses the eggs of a woman who is HIV-negative, it is still important for you to take HIV drugs to prevent passing HIV on to your child during pregnancy or childbirth.
Surrogacy
Your egg is fertilized using IVF or ICSI, then transferred to another woman's womb. That woman, the surrogate, carries and gives birth to your child. Although it is biologically possible to have the egg of a woman living with HIV fertilized by the washed sperm of a man living with HIV and implanted in an HIV-negative surrogate, you may encounter several legal or regulatory challenges to this option for getting pregnant. Even if this option is legal in your state, it may be difficult to find fertility clinics or surrogacy centers willing to provide this service to people living with HIV.
Egg Donation + Surrogacy
As a woman living with HIV, you may choose to have your partner's sperm fertilize an HIV-negative woman's egg and have that same HIV-negative woman, or another woman, give birth to your child. In this situation, your male partner's sperm would need to be washed, then used with one of the assisted reproductive techniques described above to get the HIV-negative surrogate pregnant.
Adoption
Offering a permanent family to a parentless child may be an option, whether having biologic offspring is an option for you or not. Adoptions can be done within the U.S or internationally. Unfortunately, while many people living with HIV have welcomed children into their homes through adoption, some agencies and/or countries may have prejudices against people living with HIV adopting children.
Finding a Supportive Provider
When choosing to have a child as a person living with HIV, it is important to be an advocate for yourself and your future child. Finding the right healthcare provider who is supportive of your plans to get pregnant is a big first step! A friendly healthcare provider can talk with you about many issues around pregnancy and having children: which conception option is right for you, and appropriate HIV treatments for you and/or your partner. They may also be able to speak with you about whether to disclose your HIV status to others (including other providers, your child's pediatrician, additional friends and family), and how to handle any stigma or fear you may experience around living with HIV and having a baby. Please see the main "Getting Pregnant and HIV" page for even more information about building a support network.
Ultimately, you get to choose when and whether to have children. You deserve to be treated with respect and given access to the information necessary to make an informed decision and plan for your future.
Related Resources from The Well Project
Pregnancy, Birth, and HIV (disponible en español)
HIV-Friendly Reproductive Services and Providers
Serodifferent Partners: Dating, Relationships, and Mixed HIV Status (disponible en español)
Can I Breastfeed While Living With HIV? (disponible en español)
Overview of Infant Feeding Options for Parents Living with HIV

