Para leer esta hoja informativa en español, haga clic aquí.
Note: In this fact sheet, "woman" and "man" refer to cisgender people. Much of the information for "women" is relevant to people assigned female sex at birth who do not identify as women; and the information for "men" is relevant to people assigned male sex at birth who do not identify as men.
There are several different options for reducing the chances of passing on HIV while trying to get pregnant. If you are a woman living with HIV with an HIV-negative male partner seeking information on getting pregnant, the options below might help you understand what might be best for you, and prepare you for discussions with your health care provider. (For other options and more general information, you can return to the main "Getting Pregnant and HIV" page.)
Viral Suppression of Partner Living with HIV
One of the best things that the female partner living with HIV can do in this situation is to take HIV drugs regularly and maintain an undetectable viral load (not enough HIV in her bloodstream for a test to measure). This means taking medicines even when she has no symptoms and a relatively healthy immune system.
Recent studies of gay and heterosexual ("straight") serodifferent or serodiscordant couples showed that taking HIV drugs and having an undetectable viral load reduces the risk to zero that a person living with HIV will sexually transmit HIV to their partner(s). Please see our fact sheet on Undetectable Equals Untransmittable for more information on this exciting development.
Check for STIs
Screening and treating any sexually transmitted infections or diseases (STIs or STDs) before trying to get pregnant is a great step to lower your chances of passing HIV between partners. Certain STIs can increase the chances of acquiring HIV. However, if the partner living with HIV has an undetectable viral load, the HIV-negative partner will still be protected from acquiring HIV, even if someone in the couple has an STI.
Sex without Condoms
If you choose this method, it is ideal for the partner who is living with HIV to have an undetectable viral load before the couple tries to get pregnant. This improves the mother's health and also helps to prevent HIV transmission to the baby or to her partner. Having an undetectable viral load lowers the transmission risk to a baby to less than 1 percent.
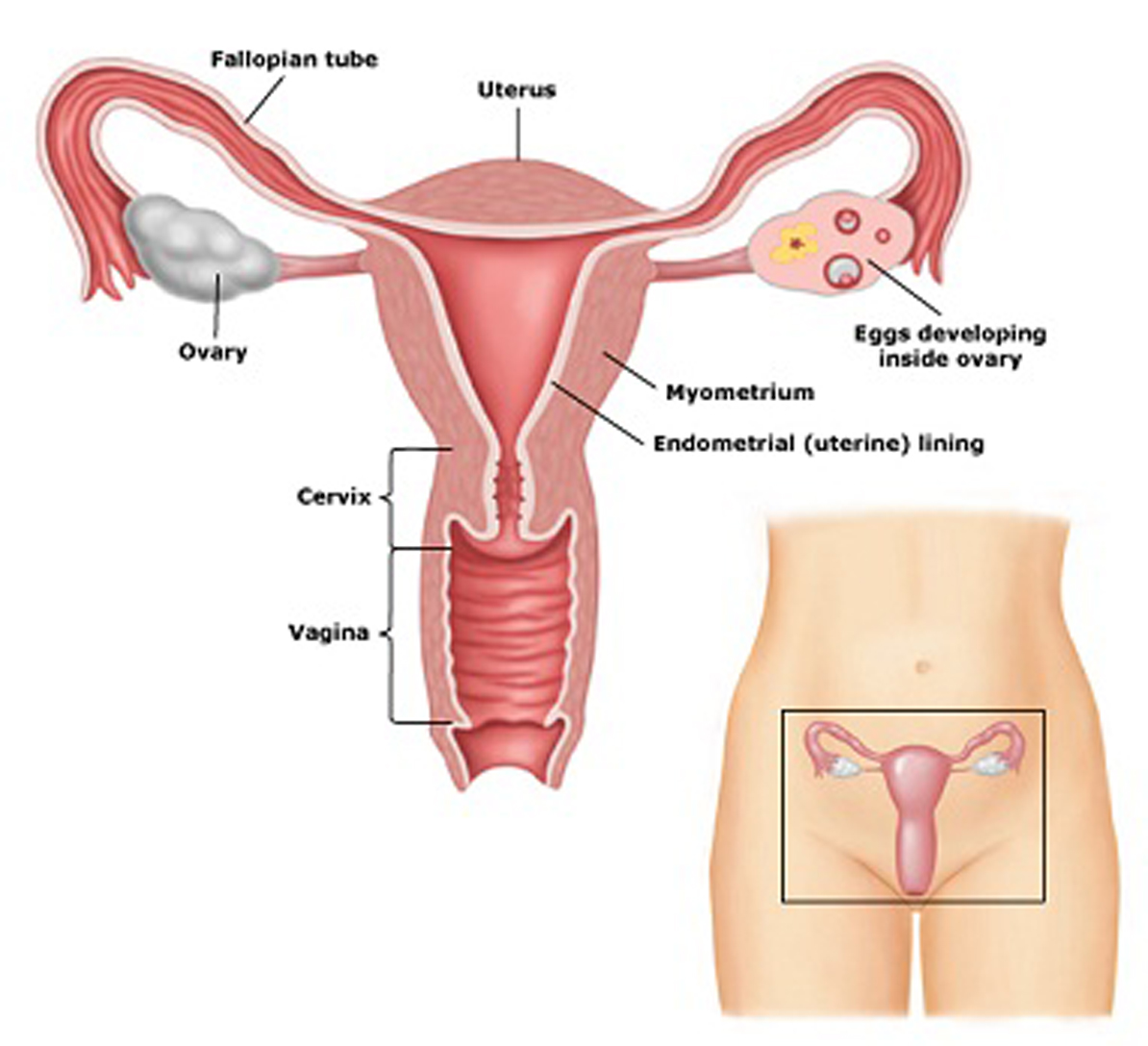
If her viral load is not known or is detectable, the risk of passing on HIV is lower if you only have unprotected sex when the woman is ovulating (when she is most likely to get pregnant; this is often called "timed intercourse"). Ovulation occurs when an egg is released from the woman's ovary, and usually happens about two weeks before a woman starts her menstrual period. Insemination during the "fertile window" – usually one to two days before ovulation and one day after ovulation – has a greater chance of success. For more information on understanding and tracking your fertility, visit:
- Home Insemination: A Guide for Women Living with HIV (PDF) (also available in Spanish)
- The Fertility Awareness Center
- Finding Your Most Fertile Days: A 3-Step Guide
Pre-Exposure Prophylaxis (PrEP)
The HIV-negative man can use Truvada (tenofovir disoproxil fumarate/emtricitabine), Descovy (tenofovir alafenamide/emtricitabine), or Apretude (cabotegravir injectable) as pre-exposure prophylaxis (PrEP). PrEP means taking HIV drugs before being exposed to HIV to prevent acquisition of the virus if the partner's viral load is unknown or is detectable. Truvada and Descovy need to be taken daily, not just right before you have sex. Apretude is injected every two months.
The US Public Health Service’s clinical practice guidelines recommend that health care providers should include PrEP in the discussion as one of the options for protecting HIV-negative partners in serodiscordant couples, particularly if they are interested in having a child. Not all health care providers are comfortable or knowledgeable about prescribing PrEP. However, you can tell your health care provider that you are interested in taking PrEP and ask them to write you a prescription for it.
If you are interested and want to learn more about PrEP, visit PleasePrEPMe.org, a growing national PrEP provider directory.
Some recent research has shown that PrEP may not add much protection when the partner living with HIV is already virally suppressed (which already lowers the risk of transmission to zero) and condomless sex is limited to the woman's fertile period.
Home Insemination
This is a cheap and simple way of getting pregnant. It involves having the man ejaculate (cum) into a clean cup or condom. If using a condom, be sure to use one without spermicide. After sex, pull the penis out of the vagina with the condom still on (you can also masturbate into a condom or cup, without vaginal sex). Then, using a syringe (without a needle), you suck up the semen and insert the syringe deep inside the vagina. Once the syringe is deep inside the vagina, you squeeze out and deposit the semen.
Based on individuals' experiences and at least one study, it is often recommended that the woman lie down for 20 minutes after inserting the semen to improve fertility. It is more effective to use this method when a woman is fertile - when she is ovulating. You can get non-needle syringes at almost any pharmacy because they are commonly used to give medicines to babies. Your HIV provider may also have some to give to you.
Assisted Reproduction
This means that a sperm fertilizes an egg with the help of a medical technique or therapy. Assisted reproduction (sometimes called "assisted reproductive technology") is useful when the future parent(s) require help to prevent HIV transmission between partners, are using donor sperm, or are having difficulty getting pregnant at home because of fertility issues. Unfortunately, few facilities offer assisted reproduction to people living with HIV, and few health insurance plans cover it. There are several types of assisted reproduction:
- Intra-vaginal insemination (IVI): Very similar to home insemination, only done in a clinic.
- Intra-uterine insemination (IUI): Semen (sperm and seminal fluid) is drawn up into a narrow tube, which is then inserted through the cervix into the uterus (womb). The semen is deposited in the uterus, where fertilization of the egg can occur.
- In-vitro fertilization (IVF): The woman takes fertility drugs to help her prepare eggs (also called ripening her eggs). When eggs are ready (or ripe), they are removed from the ovary and put in a dish with sperm. Once there is a fertilized egg (embryo), it is put back in the woman's uterus.
- Intra-cytoplasmic sperm injection (ICSI): This is a specific type of IVF in which a sperm is injected directly into an egg using a very thin needle. When a fertilized egg occurs, it is returned to the woman's uterus. This method is used when a man's sperm do not swim well or are not normally shaped.
Egg Donation
This involves using IVF and eggs donated by another woman, who is checked for fertility and diseases. The woman who is donating eggs takes fertility drugs to help her ripen her eggs. When eggs are ready (or ripe), they are removed from her ovary and put in a dish with sperm. Once there is a fertilized egg (embryo), it is put in your womb (uterus). Although this method uses the eggs of a woman who is HIV-negative, it is still important for you to take HIV drugs to prevent passing HIV on to your child during pregnancy or childbirth.
Surrogacy
Your egg is fertilized using IVF or ICSI, then transferred to another woman's womb. That woman, the surrogate, carries and gives birth to your child. If the surrogate is HIV-negative, there is zero risk of perinatal (mother-to-child) transmission of HIV. Although it is biologically possible to have the fertilized egg of a woman living with HIV implanted in an HIV-negative surrogate, you may encounter several legal or regulatory challenges to this option for getting pregnant. Even if this option is legal in your state, it may be difficult to find fertility clinics or surrogacy centers willing to provide this service to women living with HIV.
Adoption
Offering a permanent family to a parentless child may be an option, whether having biologic offspring is an option for you or not. Adoptions can be done within the US or internationally. Unfortunately, while many people living with HIV have welcomed children into their homes through adoption, some agencies and/or countries may have prejudices against people living with HIV adopting children.
Finding a Supportive Provider
When choosing to have a child as a person living with HIV, it is important to be an advocate for yourself and your future child. Finding the right health care provider who is supportive of your plans to get pregnant is a big first step! A friendly health care provider can talk with you about many issues around pregnancy and having children: which conception option is right for you, and appropriate HIV treatments for you and/or your partner. They may also be able to speak with you about whether to disclose your HIV status to others (including other providers, your child's pediatrician, additional friends and family), and how to manage any stigma or fear you may experience around living with HIV and being pregnant. Please see the main "Getting Pregnant and HIV" page for even more information about building a support network.
Ultimately, you get to choose when and whether to have children. You deserve to be treated with respect and given access to the information necessary to make an informed decision and plan for your future.
Related Resources from The Well Project
Pregnancy, Birth, and HIV (disponible en español)
HIV-Friendly Reproductive Services and Providers
Serodifferent Partners: Dating, Relationships, and Mixed HIV Status
Can I Breastfeed While Living With HIV? An Overview of Infant Feeding Options (disponible en español)