Table of Contents
- Overview
- COVID-19 Health Concerns
- COVID-19 and Women
- COVID-19 Vaccines and Treatments
- Long COVID
- COVID-19 Advocacy and Mutual Aid
- Where Are We Now?
- Taking Care of Yourself
- Honoring Community Members Lost to COVID-19
- Articles and Resources from the Early COVID-19 Pandemic
Overview
Coronavirus disease 2019, or COVID-19, is a health condition caused by a respiratory virus called SARS-CoV-2. The virus can spread (be transmitted) quickly, especially when no prevention method is in place. More than 7 million people worldwide have died of COVID-19 as of this writing.
The first cases of the novel respiratory virus emerged in Wuhan, Hubei province, China, in mid-December 2019, and the first US case was confirmed in late January 2020. By April 2020, the world had “shut down,” with travel across borders severely limited, businesses and institutions such as schools ceasing in-person operations, and most individuals who were not “essential workers” encouraged or ordered to stay home. Prevention methods such as wearing protective masks, social distancing, frequent hand-washing, and use of hand sanitizer became widespread.
Within a little over three months after the first case reports, more than 1 million people across the world had had COVID-19. However, this only included confirmed cases, likely undercounting the actual numbers. By late September 2020, more than 1 million people globally had died from COVID-19.
In record time, the virus’ genetic sequence was established, and tests, and ultimately vaccines, were developed. The first diagnostic test for the SARS-CoV-2 virus was approved in the US in early February 2020, and an at-home test became available in August 2020. Vaccine trials began in mid-March 2020 and the US approved the first COVID-19 vaccine in December 2020.
As we enter the fifth year of the pandemic, COVID-19 is still around. However, almost all measures to prevent its spread, such as masking requirements, stay-at-home orders, or mandatory vaccinations, have ended. Just like the flu, one can acquire the respiratory virus more than once. Multiple infections can cause long-term health issues. However, vaccinations and booster shots can help lessen the effects of the virus.
COVID-19 Health Concerns
SARS-CoV-2 is transmitted through droplets in the breath that enter someone else’s eyes, nose or mouth, or are breathed in. People do not need to have symptoms to pass on the virus.
As with all viruses, SARS-CoV-2 has changed over time. Some of the changes make little difference to how easily the variant (different form of the virus) spreads or how sick most people might get. Other changes more directly affect how the virus behaves among people. Some virus variants cause more severe illness than others. Even with the same variant, some people have worse symptoms than others.
Many symptoms are similar to those of an allergic reaction, a bad cold, or the flu. You can get at-home COVID-19 tests at most pharmacies, or have the government mail you some, if you live in the US. If you have any of the symptoms below and think you may have been exposed to the virus that causes COVID-19, test yourself.
Symptoms appear two to 14 days after exposure and may include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
While some people may feel only moderately sick and get through the infection on their own, others may need to see a medical provider, or even be hospitalized. If you experience any of the symptoms below, get emergency care:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake up or stay awake
- Depending on skin tone, pale, gray or blue-colored skin, lips, or nail beds
Studies have shown that women are more likely to acquire the virus, but that COVID-19 disease tends to be more severe in men. While there are some biological reasons, much of the discrepancy is related to social factors: women are more likely to be in customer-facing jobs deemed essential early in the pandemic, such as supermarket cashiers; while men are more likely to smoke, one of the risk factors for worse outcomes.
Older people and those with certain medical conditions are at greater risk of developing serious complications from COVID-19. These conditions include:
- Cancer
- Chronic kidney or liver disease
- Cardiovascular disease
- Diabetes
- Obesity
- Pregnancy
- Smoking
HIV itself increases the risk of severe COVID-19 disease but more so if HIV is not well controlled. In people living with HIV who have low viral loads and high CD4 cell counts, COVID-19 outcomes seem similar to people not living with HIV. That said, some of the conditions that increase the risk of severe disease from the respiratory virus, such as chronic kidney disease and smoking, are more common among people living with HIV than in the general population. Further, research is beginning to show a connection between living with HIV and the persistent symptoms of long COVID (discussed below).
COVID-19 and Women
Globally, 70 percent of health and social care workers are women. Many of them cared for people who had SARS-CoV-2, and protective equipment – where it existed at all – was often sized for men. This increased women’s vulnerability to the novel virus. For example, in Spain in April 2020, 76 percent of healthcare workers with COVID-19 were women.
Even before the pandemic, women performed the majority of unpaid care and domestic work. School closures and other pandemic-related shutdowns, as well as overstretched healthcare systems, only increased that burden. Lack of childcare and inability to convert their jobs to working from home forced some women to drop out of the workforce. Others lost their jobs when the businesses they worked for shut their doors for good.
Many of the jobs that cannot be done from home, such as cleaning offices, are disproportionately performed by women for low wages. Low incomes before the pandemic meant little, if any, savings once this work was no longer required. In the US, available government aid often required online application processes with lengthy delays in getting the money. It also did not reach everyone who needed it – such as people without immigration documents.
Between job losses and general lockdown orders, numerous women worldwide were stuck with partners who were already abusive – or became abusive. Some people took their stress from worries about the novel virus, lack of income, and forced togetherness out on their partners. Contacts with the US National Domestic Violence Hotline surged to unprecedented levels and several local police departments reported a 10 to 27 percent increase in domestic violence calls during stay-at-home orders.
COVID-19 Vaccines and Treatments
Medication
Most people are able to recover from COVID-19 at home, and relieve their symptoms using over-the-counter medications. If you are part of a group that is more likely to become severely ill from COVID-19, prescription treatments are available that can help lower the likelihood of being hospitalized or dying if you acquire the disease.
Groups most vulnerable to severe COVID-19 include:
- Adults 50 and over (vulnerability increases with age)
- People who have not been vaccinated or have not had boosters
- People whose immune systems are weakened
- People with conditions listed in the “Health Concerns” section above
- People living with HIV
Even if you just have mild symptoms, ask your pharmacist or healthcare provider about COVID-19 medications – and do so quickly, as treatment must start within five to seven days after symptoms appear.
Though being vaccinated lowers your likelihood of getting very sick, even vaccinated people – especially those vulnerable to severe illness – may still benefit from treatment.
COVID-19 Vaccination: On this episode of A Girl Like Me LIVE, host Ci Ci Covin talked with advocate Gina Brown, RSW, about her personal experience with the COVID-19 vaccine, clinical trials, vaccine hesitancy, and more.
View other episodes in the A Girl Like Me LIVE series
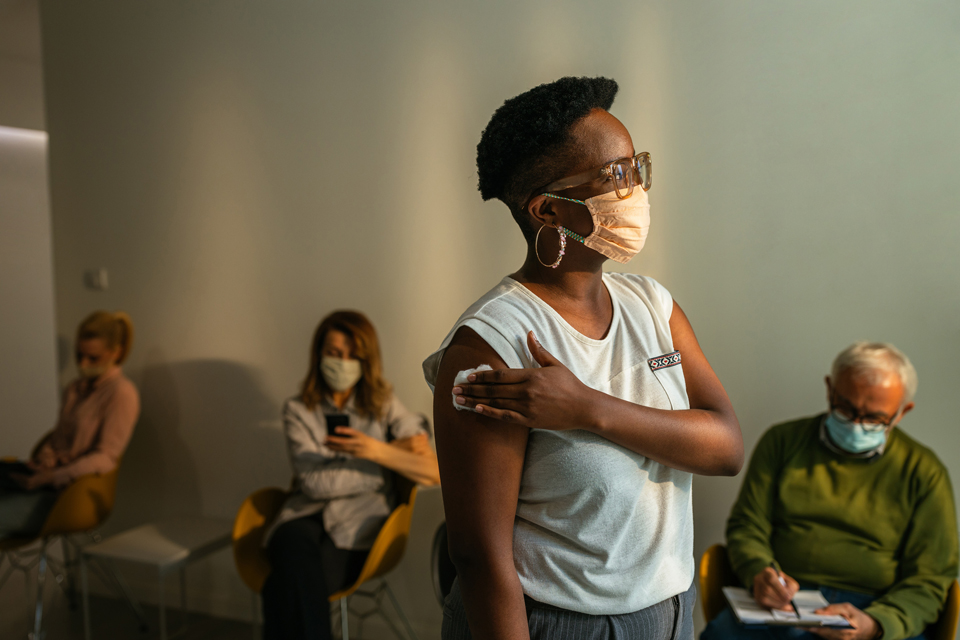
Vaccination
The basic technology behind the COVID-19 vaccine, modified ribonucleic acid (mRNA), had been in development since the 1980s. Data were also available from research into vaccines against similar viruses, such as severe acute respiratory syndrome (SARS) or Middle East Respiratory Syndrome (MERS). Using that information, several pharmaceutical companies across the world raced to develop a vaccine against the new virus, SARS-CoV-2. They were aided by increased funding for managing and containing the global pandemic.
After extensive safety testing, government agencies in various countries approved one or more vaccines for use within their borders. Booster shots for emerging new virus variants have been approved since, with the most recent round of boosters in late 2023.
While getting vaccinated may not keep you from being infected with SARS-CoV-2, it does decrease your chances of developing COVID-19, and significantly reduces the risk that you will develop severe COVID-19 disease.
According to the US Department of Health and Human Services, anyone older than 6 months can get the COVID-19 vaccine for free, even if they do not have health insurance or immigration documentation in the US. Early in the pandemic, all pharmacies offered the shots for free. Now not all pharmacies participate in the government program, and those that don’t may bill people who don’t have insurance.
Because the vaccines were developed so quickly and used novel technology, some people were skeptical that they would work and were safe. Conservative groups and politicians fanned that distrust, and both misinformation (incorrect information passed on because the person doesn’t know better) and disinformation (incorrect information passed on intentionally for a specific purpose) around COVID vaccination began to flourish.
It is important to note that, while both infection and vaccination produce antibodies against SARS-CoV-2, the antibodies generated by vaccination are longer-lasting and more predictable. SARS-CoV-2 keeps changing (mutating) because that’s what viruses do, not because of the vaccine. Vaccine ingredients are safe. Health events reported to the US Vaccine Adverse Event Reporting System, which monitors vaccine safety, are often sent in by laypersons, not healthcare providers. What they report may not be related to the vaccination at all.
Long COVID
In early October 2021, the World Health Organization published a definition of a condition that has become known as long COVID – symptoms such as persistent fatigue, muscle aches, shortness of breath, and memory issues after having COVID-19. Symptoms differ among people and can include ongoing fever, sleep problems, long-lasting change in smell or taste, gut issues, a rash, or other conditions.
Long COVID is still poorly understood. Much of pandemic-related research was dedicated to preventing and treating the acute illness, with much less attention paid to long-term consequences for some people. Broader research into long COVID is now getting underway. Results from some studies are already showing a connection between long COVID and HIV. One large study found that people living with HIV were approximately 30 to 80 percent more likely to experience prolonged symptoms after having COVID-19, with the chance even higher among people who acquired strains of SARS CoV-2 before mid-2021.
In the early days of the HIV epidemic, activists pushed for research to understand the then-new virus and find treatments for its long-term effects. They also fought against stigma and for social and financial support for people living with HIV. HIV activists are now using the experience from those struggles to build a movement advocating for research and supports for people with another chronic illness, long COVID.
COVID-19 Advocacy and Mutual Aid
Shutdowns started in the US in mid-March 2020. By early May, the unemployment rate had hit almost 15 percent. Many of the 20.5 million people who lost their jobs had worked in the hospitality or leisure industries, often for low wages. In response, the US government sent “economic impact payments” to low- and middle-income US citizens and permanent residents who had filed a tax return. Many of the people who most needed the money – such as those with another immigration status, or who had not filed tax returns for lack of income – were left out.
In early October 2020, 52 million people in the US were food insecure. In response, local groups built “little free pantries” – modeled after little free libraries – and established “community fridges.” Neighbors filled these with groceries or home-cooked meals, and people took what they needed to feed themselves and their families. The pantries were also used to redistribute free COVID-19 tests and other supplies to people who could not get them – e.g., because they were unhoused. Many pantries and fridges continue to exist to this day.
Local mutual aid groups arranged for volunteers to go shopping or run errands for people vulnerable to severe effects from COVID-19. Volunteers also distributed hot meals and took people to vaccination or testing sites. Some of these efforts continue to support people with long COVID.
Surges in protests around the Black Lives Matter movement and other social justice issues also occurred in the summer of 2020, during the height of the pandemic. Despite large marches, there was no significant increase in COVID-19 cases because demonstrators took virus precautions: masks, hand sanitizer, social distancing. At some of the larger events, volunteers handed out these and other supplies, as well as information on keeping safe at protests.
COVID-19 Vaccination and Clinical Trials: View this informative and engaging conversation with A Girl Like Me LIVE host Ci Ci Covin, physician and advocate Oni Blackstock, MD, and The Well Project CAB chair Gina Brown, RSW, covering the COVID-19 vaccine, clinical trials, and more to know to keep safe.
View other episodes in the A Girl Like Me LIVE series
Where Are We Now?
After initial lockdowns and massive efforts to prevent the spread of the pandemic, many governments, including the US, have declared the emergency over. However, the virus that causes COVID-19 is still in circulation and continues to cause illness and death worldwide, if not at the scale experienced in 2020.
When most people stopped masking, getting COVID-19 booster shots, observing a safe distance from others, or staying home when sick, some people with long COVID or at risk of severe complications from the respiratory virus could no longer safely leave home.
HIV activists have successfully pushed for safety protocols around handling blood, such as wearing a mask and gloves when tending to an injured person, to become a universal practice. Similarly, wearing masks – especially in medical settings or when someone has any respiratory symptoms – frequent hand washing, and staying home when sick could become universal precautions that would allow people vulnerable to COVID-19 and other respiratory illnesses to enjoy public settings again.
Taking Care of Yourself
Anyone at any age can acquire, become sick from, and potentially even die of COVID-19. Older adults and people with preexisting conditions and vulnerabilities may be more likely to experience severe illness. Keeping up to date with vaccinations, and taking treatment if appropriate, lowers the chance of severe illness. You can also reduce the spread of COVID-19 – and your own chance of getting COVID – by taking precautions like:
- keeping your hands clean and/or sanitized;
- wearing a mask (masking up) in places where you will be close to others for a while without air flowing through (ventilation);
- getting tested if you have symptoms or contact with someone who has COVID; and
- staying home if you are sick.
Honoring Community Members Lost to COVID-19
Tributes to HIV/AIDS Community Members We've Lost to COVID-19 So Far (TheBody): Slideshow commemorating folks who have died of COVID-19 who were living with HIV, working in the field, and/or addressing HIV in media, art, and culture. Author Tim Murphy asks those who know others in the HIV community who passed away from COVID-19 to email him.

Our Community Champion, Deloris Dockrey (ICW, GNP+, PWN-USA): Dockrey was a ray of light and positivity, as well as a fierce advocate for the rights of people living with HIV, especially women.

R.I.P. Lorena Borjas, a Transgender Latinx Activist Lost to COVID-19 (POZ; includes video): Borjas fought tirelessly for transgender and immigrant communities in New York City, operating HIV-testing programs and syringe exchanges and fighting to change police policies toward trans people and sex workers.
Articles and Resources from the Early COVID-19 Pandemic
From mid-March 2020 through September 2021, The Well Project maintained a comprehensive list of trusted resources we believed could be useful to our community – including women living with HIV, their allies, and healthcare providers – during a difficult and disorienting time. We have kept some of these articles and resources on our website as an archive of materials from this period in our community’s history. Any basic information mentioned on pages and in videos is likely to be out of date.